Previous issue | Next issue | Archive
![]() Volume 13 (3); September 25, 2023
Volume 13 (3); September 25, 2023
| Morphometric and microbiological features of ventilator associated tracheobronchitis |
Research Paper
Morphometric and microbiological features of ventilator associated tracheobronchitis
Ibadov RA, Azizova GM, Ibragimov SK.
J. Life Sci. Biomed., 13(3): 48-52, 2023; pii:S225199392300007-13
DOI: https://dx.doi.org/10.54203/jlsb.2023.7 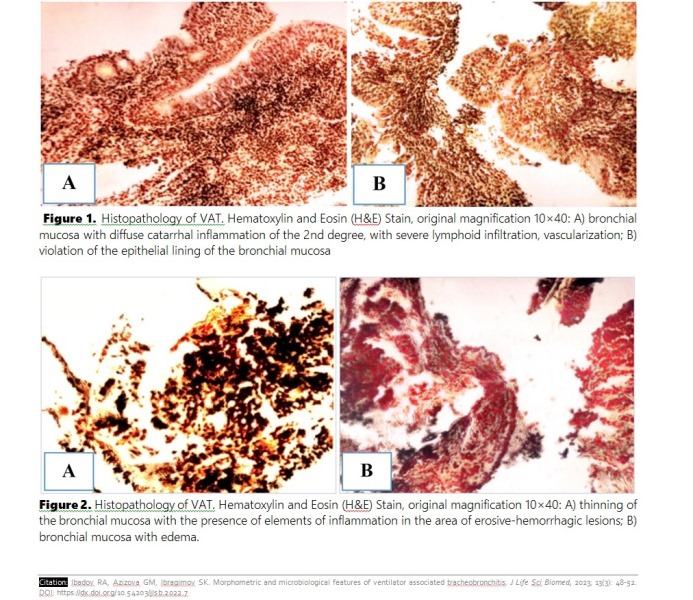 Abstract
Abstract
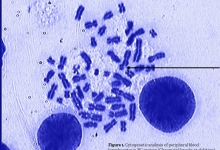
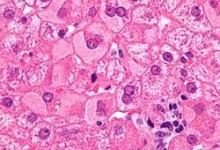
Changes in the composition of the microbiota of the tracheobronchial tree in patients on prolonged mechanical ventilation can contribute to various disorders of the immune defense of the respiratory tract, damaging mucociliary clearance, and cause a strong inflammatory response, including the formation of ventilator-associated tracheobronchitis (VAT). The aim was to study the specifics of changes in the microflora and histopathology of the tracheobronchial tree in VAT. Over a 10 year period 975 bacteriological analyzes were carried out in 355 patients who were on extended mechanical ventilation for more than 48 hours. VAT is accompanied by a pronounced lymphoid-neutrophilic infiltration of the mucosa of the trachea and bronchi, and in a complicated course with the presence of a purulent-inflammatory and erosive-hemorrhagic component leads to a violation of the integrity of tissues due to destruction and necrosis. The leading pathogens were representatives of gram-negative flora of 65.8% (47-76%), gram-positive flora was detected in 17.5% (10-30%) of cases, fungi of the genus Candida in 16.5 (4-42%) cases. Analysis of the antibiograms of isolated cultures in patients on prolonged mechanical ventilation shows high resistance to a wide range of antibiotics, namely: acinetobacter spp. - high resistance to all antibiotics, except for imipenem (0% resistant strains), polymyxin (0%) and tetracyclines (7-15.4%). Imipenem (10.5%), polymyxin (10.5%), amikacin (31.5%) and cefoperazone/sulbactam (31.5%) are active against Esherichia coli. Klebsiella pneumoniae was susceptible to imipenem, amikacin, ofloxacin and inhibitor-protected antibiotics-cefoperazone/sulbactam, piperacillin/tazobactam. Staphylococcus aureus was susceptible to III generation cephalosporins (cefotaxime, ceftriaxone, cefoperazone) and tetracyclines - 36.3% of resistant strains. Microbiological monitoring in patients with VAT over a 10-year period revealed a trend towards the prevalence of gram-negative microflora inoculation, and over the past two years, the range of isolated multi-resistant flora has been expanding.
Keywords: Prolonged mechanical ventilation, Nosocamial infection, Ventilator associated tracheobronchitis, Microbiology, Histopathology
[Full text-PDF] [ePub] [Export citation from ePrint] [How to Cite]
| COVID-19-induced cardiovascular complexities |
Research Paper COVID-19
COVID-19-induced cardiovascular complexities
Ibadov RR, Akilov KA, and Ibragimov SK.
J. Life Sci. Biomed., 13(3): 53-58, 2023; pii:S225199392300008-13
DOI: https://dx.doi.org/10.54203/jlsb.2023.8 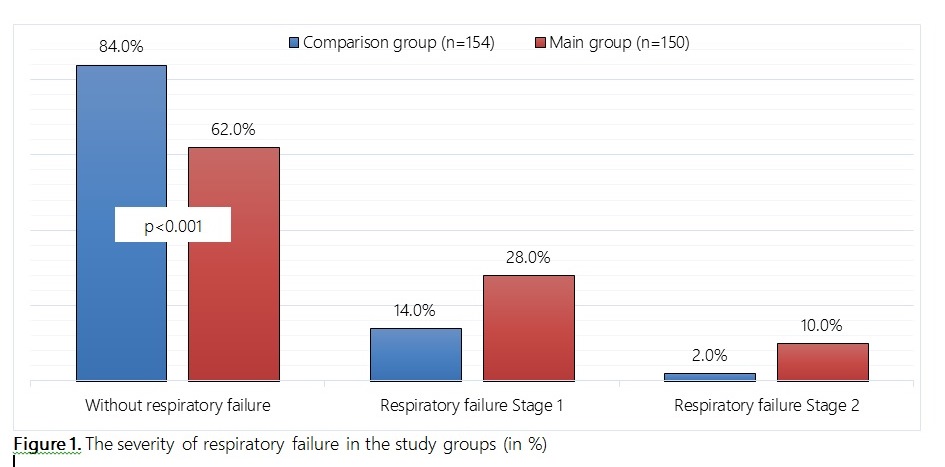 Abstract
Abstract
This study aimed to investigate the features of the clinical course of COVID-19 in combination with the pathology of the cardiovascular system (CVS). A prospective study was carried out. The main group (n=150) consisted of patients with changes in the cardiovascular system associated with COVID-19, i.e. newly diagnosed CV pathology, and patients with exacerbation of cardiac pathology against the background of COVID-19. The comparison group (n=154) included patients with COVID-19, but without any significant concomitant cardiac pathology. The average age of patients in the main group was 67.7 years (from 47 to 86 years), in the comparison group of 66.1 years (from 48 to 88 years). The study groups were representative and did not differ statistically in the nature of COVID-19 symptoms and the degree of lung involvement. Among the cardiac pathology, progressing or first occurring against the background of infection with COVID-19, in most cases, arterial hypertension of II-III degree (60.0%), coronary heart disease (48.7%), arrhythmias (23.3%) were diagnosed. Echocardiographic abnormalities included right ventricular dysfunction (22.7%), left ventricular contractility disorders (18.7%), with decreased ejection fraction (17.3%), diastolic dysfunction (14.0%), and toxic myocarditis (7.3%). The most significant risk factors were the presence of a burdened medical history (RR=10.39), elevated body mass index over 30 (RR=2.63) and diabetes mellitus (RR=1.55). In patients with COVID-19 in combination with CVS pathology, a relatively high incidence of acute onset (64.0% vs. 44.2%; p<0.001), respiratory failure (83.7% vs. 62.0%; p<0.001), admission to the intensive care unit (25.3% vs. 11.7%; p=0.004), development of acute respiratory distress syndrome (20.0% vs. 9.1%; p=0.012), hospital mortality (10.7% vs. 2.7%; p=0.006). Cardiac manifestations of COVID-19 included focal or global myocardial inflammation, ventricular dysfunction, heart failure, and arrhythmias. A high frequency of acute onset of the disease, respiratory failure and hospital mortality is determined.
Keywords: COVID-19, SARS-CoV-2, cardiovascular system, clinical course, comparative analysis
[Full text-PDF] [ePub] [Export citation from ePrint] [How to Cite]
Previous issue | Next issue | Archive
![]() This work is licensed under a Creative Commons Attribution 4.0 International License (CC BY 4.0)
This work is licensed under a Creative Commons Attribution 4.0 International License (CC BY 4.0)